Is Obesity a Disease?
Well, back in 2013 the American Medical Association (AMA) decided that obesity met all the requirements of a Disease, and therefore now classifies obesity as a Disease.
Follow the Money
I must admit that my cynical side (all of me really) wondered why the AMA would fall on that side of the fence, when most people in the streets regard obesity as the sign of overeating. Even now, 7 years later that is still the case.
Did the declaration of the AMA mean that the bureaucrats immediately declared a war on obesity similar to the one that Nixon declared on Cancer back in December 23, 1971? [The signing of the National Cancer Act by President Richard M. Nixon on December 23, 1971, was considered a declaration of War on Cancer (although researchers had never slowed in their efforts to combat this multi headed disease). The law earmarked $1.5 million for cancer research over a 3-year period and broadened the scope and responsibilities of the National Cancer Institute. Equally important, the law designated the fight against cancer a national priority.]
In fact at the time (1971) the copy read, "Dr. Sidney Farber, Past President of the American Cancer Society, believes: 'We are so close to a cure for cancer. We lack only the will and the kind of money and comprehensive planning that went into putting a man on the moon'."[1] [In reality, the War on Cancer has turned into a Cash Cow for all parties involved with Cancer, and it is unlikely that this war will ever be won by the human race. There is just too much money involved to justify finding a real solution.]
So here we are some 48 years later with no end in sight for the demise of Cancer in any form using the treatments approved by the AMA and FDA, and they now add another disease - obesity to the ever growing list of human ailments.
This is partly due to the fact that the Medical Industry was now able to claim weight loss clinics and methods as part of their domain. This is especially true when you realise that the weight loss industry as a whole was a $64 billion market in 2014.[2] Purely from a "follow the money" outlook this large non-medical market was too tempting for the AMA to ignore.
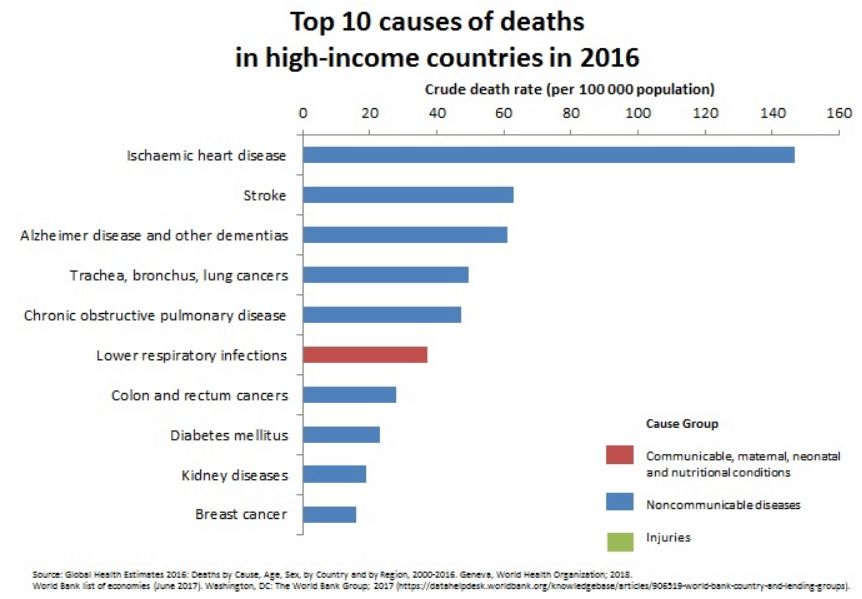
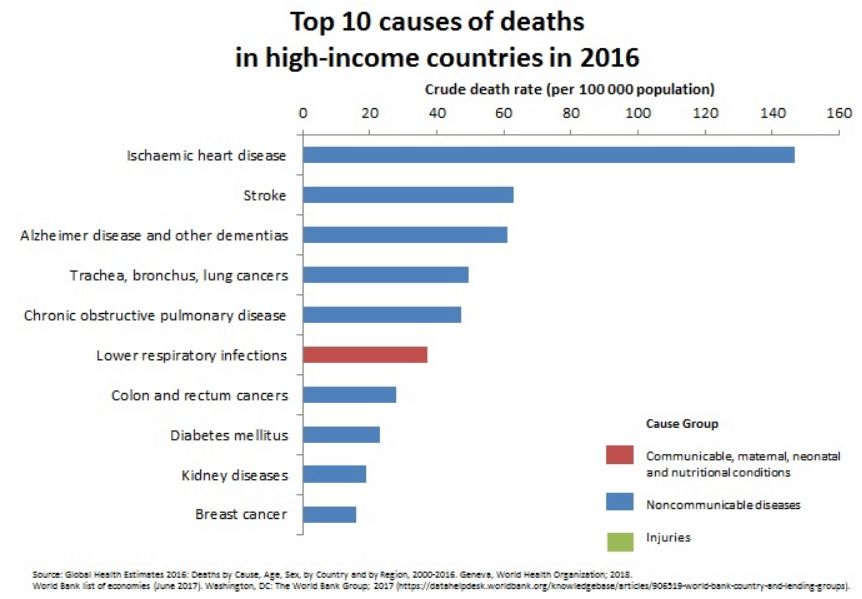
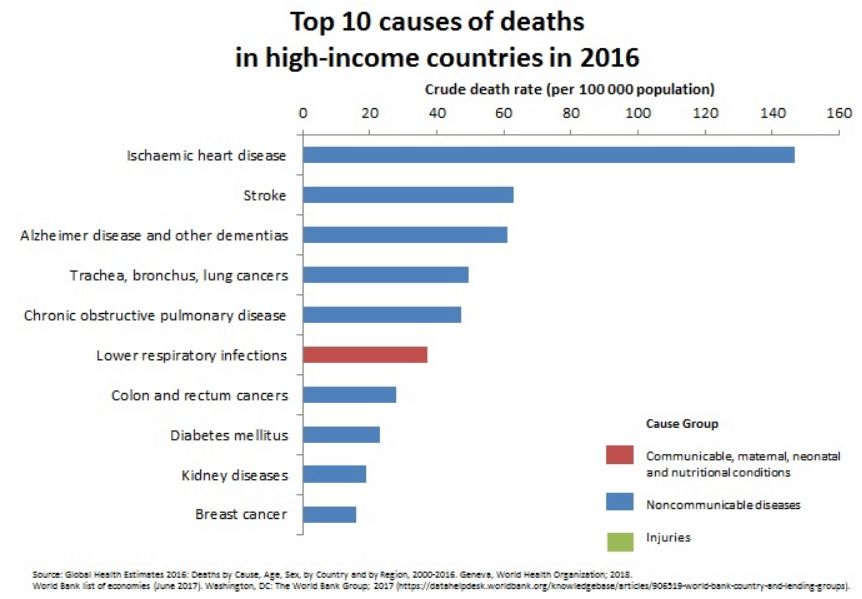
9 out of 10 of the causes of death in high income countries are related to being overweight, obese or morbidly obese. These are preventable.
All of the blue causes of Death shown opposite are the result of being obese or even overweight.
Obesity was declared a disease so the Medical Industry could get involved in the $64 billion (2014) weight loss market.
What was the reasoning behind the AMA making this decision?
It is interesting to note that in the meeting minutes the A.M.A. House of Delegates voted AGAINST the conclusions of the association’s Council on Science and Public Health, which had studied the issue over the last year. The council said that obesity should not be considered a disease mainly because the measure usually used to define obesity, the body mass index (BMI), is simplistic and flawed.
Some people with a B.M.I. above the arbitrary level that usually defines obesity are perfectly healthy while others below it can have dangerous levels of body fat and metabolic problems associated with obesity. [There is no indication of any scientific reason why the BMI levels defining overweight, obese or morbidly obese are set at these levels. I have been unable to find any studies that support these numbers, and I feel that they are just arbitrary numbers pulled out of the air by the initial publisher of the BMI.]
“Given the existing limitations of B.M.I. to diagnose obesity in clinical practice, it is unclear that recognizing obesity as a disease, as opposed to a ‘condition’ or ‘disorder,’ will result in improved health outcomes,” the council wrote. [This has been shown to the case as now 50% of EU citizens and 2/3 of the USA population are defined as obese. This just makes the market for weight loss and obesity clinics manned by members of the AMA to make even more money.]
The council summarized the arguments for and against calling obesity a disease.
One reason in favour, it said, was that it would reduce the stigma of obesity that stems from the widespread perception that it is simply the result of eating too much or exercising too little. Some doctors say that people do not have full control over their weight.
Supporters of the disease classification also say it fits some medical criteria of a disease, such as impairing body function. [So does losing a limb, but that isn't classed as a disease, yet.]
Those arguing against it say that there are no specific symptoms associated with it and that it is more a risk factor for other conditions than a disease in its own right.
They also say that “medicalizing” obesity by declaring it a disease would define one-third of Americans as being ill and could lead to more reliance on costly drugs and surgery rather than lifestyle changes. [They got the numbers wrong on that as it is now 2/3 of Americans are classified as obese.]
Some people might be overtreated because their B.M.I. was above a line designating them as having a disease, even though they were healthy.
The delegates rejected the conclusion of the council and voted instead in favour of a resolution pushed by the American Association of Clinical Endocrinologists, the American College of Cardiology and some other organizations. [The fix was obviously in as the rejection of a special council who studied the obesity problem for over a year was thrown out in favour of chasing the $64 billion weight loss market [2] that the Doctors were not currently involved in at a single meeting.]
This resolution argued that obesity was a “multi metabolic and hormonal disease state” that leads to unfavorable outcomes like Type 2 diabetes and cardiovascular disease.
“The suggestion that obesity is not a disease but rather a consequence of a chosen lifestyle exemplified by overeating and/or inactivity is equivalent to suggesting that lung cancer is not a disease because it was brought about by individual choice to smoke cigarettes,” the resolution said. [Once again this comment is self serving as you do not need to be a smoker to get lung cancer. See Lung Cancer article here.]
Eating more calories than you burn in daily activity and exercise (on a long-term basis) causes obesity. Over time, these extra calories add up and cause you to gain weight.
Eating more calories than you burn in daily activity and exercise (on a long-term basis) causes obesity. Over time, these extra calories add up and cause you to gain weight.
You see this shown again and again when you see malnourished or starving people - none of these people are obese or even overweight.
Common specific causes of obesity include:
Certain medical conditions may also lead to weight gain. These include:
Who is at risk for obesity?
Basically, anyone - man, woman and child are all at risk from becoming obese. This is especially true if they indulge in any of the actions mentioned above. The main ones are eating fatty foods (fast food is the greatest contributor), processed food and not doing any exercise, such as walking for 30 - 60 minutes a day. TV, Video games and always going everywhere by car instead of walking or using a bicycle also do not help.
According to the Food Research & Action Center - and everyone else - more than 2/3 of Americans and 50% of EU citizens are overweight or obese. Two decades ago that was only ¼ of the population. Put simply, significantly more people should be losing weight. The difference, however, between now and 20 years ago is a change in focus away from deprivation dieting to a more holistic, healthy lifestyle all the time. Instead of saying, “I’ve got to lose this extra weight right now,” people are saying “I’ve got to live a healthier life.” Folks that were dieting are at least trying to eat fresher, greener foods, exercise more regularly and in general take better care of themselves. An interesting statistic to illustrate the point: a whopping 77% of Americans claim to be trying to eat healthier - against the 19% that claim to be on a diet.
Physicians and health insurance providers are not shy about pitching weight loss as preventative health care. Medical weight loss plans as a niche weight loss business have been making a lot of money and likely will into the future.
73% of men in the United States are overweight, compared to only 63% of women. But memberships in weight loss programs are dominated by women - an estimated 90% of Weight Watchers members are women. The discussion about why can be long and varied - and controversial at points - but the fact remains: men are overweight and have still barely been touched by weight loss services.
Genetics
Some people possess genetic factors that make it difficult for them to lose weight. This group is a very small proportion of the population and does not include 2/3 of the people in the USA or EU. The Medical Industry would like you to believe that being overweight or obese in your case is genetic and should be dealt with solely by Doctors. Unless you suffer from any of the 5 medical conditions shown above then there is a 99% chance that being overweight or obese is a personal choice determined by what you put in your mouth.
Environment and Community
Your environment at home, at school, and in your community, can all influence how and what you eat and how active you are. Maybe you haven’t learned to cook healthy meals or don’t think you can afford healthier foods. If your neighborhood is unsafe, maybe you haven’t found a good place to play, walk, or run.
If this is your problem then join our 7 day and 30 challenge to start you on your way. While we can support you in helping yourself by supplying recipes, food lists, and exercise suggestions we cannot do it for you. Moving through these courses will give you the confidence which will change your life for the better.
Psychological and other factors
Depression can sometimes lead to weight gain, as people turn to food for emotional comfort. Certain antidepressants can also increase risk of weight gain. Check out the list here to find out if your prescription is part of the weight gain problem. If it is then ask your Doctor to change your medication.
Smoking
It’s a good thing to quit smoking, but quitting can also lead to weight gain. For that reason, it’s important to focus on diet and exercise while you’re quitting.
Medication
Medications such as steroids or birth control pills can also put you at greater risk for weight gain. Check with your Doctor to find out if that is part of the weight problem.
How is Obesity diagnosed?
Supplied by BMI Calculator USA
Most times the Doctor or Nurse will measure how big you are around your stomach, take your weight and your height.
They then will check the BMI [3] Obesity charts. Calculate your own BMI on the left.
Obesity is defined as having a BMI of 30 or more. Body mass index is a rough calculation of a person’s weight in relation to their height.



Other more accurate measures of body fat and body fat distribution include skinfold thickness, waist-to-hip comparisons, and screening tests such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) scans.
Your doctor may also order certain tests to help diagnose obesity as well as obesity-related health risks. These may include blood tests to examine cholesterol and glucose levels, liver function tests, diabetes screen, thyroid tests, and heart tests, such as an electrocardiogram.
A measurement of the fat around your waist is also a good predictor of risk for obesity-related diseases.
When you get the bill for all these tests you might begin to understand why the AMA wanted to declare Obesity as a Disease.
What are complications of obesity?
Obesity leads to much more than simple weight gain. Having a high ratio of body fat to muscle puts strain on your bones as well as your internal organs. It also increases inflammation in the body, which is thought to be a cause of cancer. Obesity is also a major cause of type 2 diabetes.
Obesity has been linked to a number of health complications, some of which are life-threatening:
How is obesity treated?
If you’re obese and haven’t been able to lose weight on your own, medical help is available. In addition there are a number of of Weight Loss Clinics that will work with you (for a fee) to support you in losing weight. Most of these tend to be food based - i.e. buy our food and lose weight.
Start with your family physician who may be able to refer you to a weight specialist in your area.
Your doctor may also want to work with you as part of a team helping you lose weight. That team might include a dietitian, therapist, and/or other healthcare staff.
Your doctor may work with you on making lifestyle changes. It is most likely that they will recommend medications or weight loss surgery as well.
Lifestyle and behavior changes
Your healthcare team or Weight Loss Clinic can educate you on better food choices and help develop a healthy eating plan that works for you. A structured exercise program and increased daily activity — up to 300 minutes a week — will help build up your strength, endurance, and metabolism.
Counseling or support groups may also identify unhealthy triggers and help you cope with any anxiety, depression, or emotional eating issues.
Medical weight loss
Your doctor may also prescribe certain prescription weight loss medications in addition to healthy eating and exercise plans. Medications are usually prescribed if other methods of weight loss haven’t worked and if you have a BMI of 27 or more in addition to obesity-related health issues.
Prescription weight loss medications either prevent the absorption of fat or suppress appetite. These drugs can have unpleasant side effects. For example, the drug orlistat (Xenical) can lead to oily and frequent bowel movements, bowel urgency, and gas. Your doctor will monitor you closely while you’re taking these medications.
Weight loss surgery
Weight loss surgery (commonly called “bariatric surgery”) is the prefered option in the USA as it does not require a commitment from patients that they will change their lifestyle. Surgery forces the patient to change their lifestyle and food intake, otherwise the patient is likely to die when the internal surgery ruptures.
These types of surgery work by limiting how much food you can comfortably eat or by preventing your body from absorbing food and calories. Sometimes they do both. It does not rely on the willpower of the patient to eat less.
Weight loss surgery isn’t a quick fix. It’s a major surgery and can have serious risks. After surgery, patients will need to change how they eat and how much they eat or risk getting sick or dying.
Candidates for weight loss surgery may have a BMI of 40 or more, or have a BMI of 32 to 39.9 along with serious obesity-related health problems.
Patients will often have to lose weight prior to undergoing surgery. Additionally, they will normally undergo counseling to ensure that they’re both emotionally prepared for this surgery and willing to make the necessary lifestyle changes that it will force on them.
Surgical options include:
What is the long-term outlook for obesity?
There’s been a dramatic increase in obesity and in obesity-related diseases. This is the reason why communities, states, and the federal government are putting an emphasis on healthy food choices and activities to help turn the tide on obesity.
Ultimately, however, the responsibility is on each of us to make these healthy changes.
How can you prevent obesity?
Help prevent weight gain by making good lifestyle choices. Aim for moderate exercise (walking, swimming, biking) for 20 to 30 minutes every day.
Eat well by choosing nutritious foods like fruits, vegetables, whole grains, and lean protein. Eat high-fat, high-calorie foods in moderation.
Risks
The weight loss business is an industry fraught with misinformation. False claims about potential results and benefits run rampant. In the last decade alone the Federal Trade Commission has brought more than 80 law enforcement actions against companies making deceptive weight-loss claims. For patients considering joining a weight loss clinic it’s important to understand how and why it does what it claims to do - and if it really does it!
Do-it-yourself diets have also stormed onto center stage. From Atkins to South Beach to eating like a caveman - and a thousand others - diet information is easier to find than ever. Online support communities offer many of the benefits of in-person support, but have the added benefit of anonymity.
The number of bariatric surgeries have increased by 10% in the last decade alone. This surgery reduces the size of the stomach and has been an effective weight loss technique - without a lot of the work required the old fashioned way.
No matter what type of solution you you pick to stop you being overweight or obese - it all come down to one thing - less food in and weight goes down. Check out our 7 and 30 day challenges.
Fact Checked References
1. Mukherjee S. A moon shot for cancer. In: The Emperor of All Maladies: A Biography of Cancer. New York: Scribner; 2010: 180.
2. MarketResearch.com: The U.S. Weight Loss and Diet Control Market (11th Edition)
3. https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
CDC.gov: Adult Obesity
Healthy People.gov: Archive
Adult obesity facts. (2018).
cdc.gov/obesity/data/adult.html
Body mass index: Considerations for practitioners. (n.d.).
cdc.gov/obesity/downloads/bmiforpactitioners.pdf
Child obesity facts: Prevalence of childhood obesity in the United States. (2018).
cdc.gov/obesity/data/childhood.html
Facts and statistics: Physical activity. (2017). https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html
F as in fat: How obesity threatens American’s children. (n.d.). https://www.rwjf.org/content/dam/farm/reports/reports/2010/rwjf62003
Guo X, et al. (2017). High fat diet alters gut microbiota and the expression of paneth cell-antimicrobial peptides preceding changes of circulating inflammatory cytokines. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5339499/
Hall KD, et al. (2016). Calorie for calorie, dietary fat restriction results in more body fat loss than carbohydrate restriction in people with obesity. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4603544/
Mayo Clinic Staff. (2015). Obesity.
mayoclinic.org/diseases-conditions/obesity/symptoms-causes/syc-20375742
Mayo Clinic Staff. (2018). Cushing’s syndrome.
mayoclinic.org/diseases-conditions/cushing-syndrome/symptoms-causes/syc-20351310
Mayo Clinic Staff. (2018). Hypothyroidism (underactive thyroid).
mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284
Mayo Clinic Staff. (2018). Prader-Willi syndrome.
mayoclinic.org/diseases-conditions/prader-willi-syndrome/symptoms-causes/syc-20355997
Obesity. (n.d.).
endocrinefacts.org/health-conditions/obesity/
O’Neill AM. (2016). High-fat Western diet-induced obesity contributes to increased tumor growth in mouse models of human colon cancer. https://www.ncbi.nlm.nih.gov/pubmed/27866828
Polycystic ovary syndrome. (n.d.).
ncbi.nlm.nih.gov/pubmedhealth/PMHT0024506/
Position of the American Dietetic Association: Fat replacers. (2005). https://jandonline.org/article/S0002-8223(04)01853-X/fulltext


[…] percentage and are classified as overweight. 1/3 of all Americans are obese, which is defined as a Body Mass Index (BMI) of over 30. This includes 1 in 6 children being clinically obese. This is a serious health crisis, […]